What Are the Signs of Childhood Trauma in Adults?

Childhood trauma leaves fingerprints. They aren't always visible, nor are they always remembered, but they’re always felt. It can shape everything from the way we breathe through conflict and choose partners, to how we react to disappointment, or handle silence.
Even when memories stay buried, the body lives the story. Stephen Porges, the neuroscientist behind the Polyvagal Theory, explains that the nervous system learns to prioritize survival long before the brain can comprehend danger. A child who grows up in fear learns to live in a state of fight, flight, or freeze.
So when adulthood arrives, many people aren’t reacting to the present moment; they’re responding to a nervous system still calibrated to the past.
Millions carry these invisible echoes. The National Center for PTSD notes that exposure to traumatic experiences in early childhood is widespread. Many children experience physical abuse, sexual abuse, neglect, natural disasters, loss, or other adverse childhood experiences. Some later develop post-traumatic stress disorder, while others show signs of unresolved trauma, emotional numbness, anxiety disorders, mental illness, or persistent anxiety.
Understanding the signs of childhood trauma in adults isn’t about assigning blame. It’s about clarity — and clarity is the first step toward healing.
Key Learnings
- Childhood trauma wires the nervous system for survival, shaping emotional regulation, anxiety symptoms, relationships, and physical symptoms.
- Signs show up emotionally, physically, behaviorally, and relationally, often long before a person connects them to repressed childhood trauma.
- Trauma is both psychological trauma and physiological, as explained by psychologists Peter Levine, Gabor Maté, and Bessel van der Kolk.
- Healing is possible through therapy, somatic practices, emotional tracking, and a personalized healing plan for childhood trauma.
How Childhood Trauma Echoes Through Adult Life
When a child experiences overwhelming stress without support, the body perceives the experience as a threat. Peter Levine, founder of Somatic Experiencing, explains that trauma is stored in the body as incomplete survival responses.
If those responses never complete — running, crying, shaking, reaching for a caregiver — they get trapped. Years later, they show up as emotional dysregulation, physical health conditions, anxiety disorders, or repressed memories.
This is why childhood trauma survivors often don’t recall the traumatic childhood memories but still display childhood trauma symptoms that affect a person’s everyday life, from difficulty maintaining healthy relationships to emotional shutdown.
Bessel van der Kolk writes in The Body Keeps the Score that trauma lives “not as a story but as a state.”
It’s essential to recognise that childhood trauma doesn’t always look like a single dramatic event. It can be the absence of nurturing, attunement, or consistent emotional safety, or a series of small adverse experiences over time. These kinds of developmental traumas quietly erode a child’s sense of safety, self-regulation, and attachment to others. As research on developmental trauma shows, repeated emotional neglect or inconsistent caregiving can shape the nervous system just as profoundly as overt abuse or catastrophic events.
Trauma Triggers in Adulthood
Triggers are reminders, internal or external, that reactivate stored stress responses. They may lead to intrusive memories, emotional flashbacks, panic, or avoidance.
| Internal Triggers | External Triggers |
|---|---|
| fear | conflict |
| loneliness | trauma anniversaries |
| muscle tension | certain smells or sounds |
| emotional numbness | reminders of child abuse or childhood abuse |
| chronic pain | stories about traumatic experiences |
| sleep disturbances | |
| heightened sensitivity |
Gabor Maté’s trauma research emphasizes that these are not personality flaws; they’re physiological responses shaped by early environments.
Emotional Signs of Childhood Trauma in Adults
Anxiety Disorders and Hypervigilance
Growing up with unpredictable caregivers or experiencing childhood trauma can keep the nervous system stuck in fight-or-flight. Adults may experience:
- worry that doesn't match the situation
- racing thoughts
- panic symptoms
- chronic stress
- trouble relaxing
- sleep disturbances
These patterns can resemble generalized anxiety disorder and often overlap with mental disorders triggered or worsened by early adverse experiences.
Depression and Emotional Numbness
When a child cannot escape danger, the body often enters a state of shutdown. This adult pattern is linked to:
- disconnection
- loss of interest
- chronic exhaustion
- emotional numbness
- difficulty feeling joy
Low Self-Esteem and Chronic Shame
Children assume everything is their fault.
Adults carry that forward as:
- “I’m not enough.”
- “I shouldn’t take up space.”
- “People always leave.”
Chronic shame is one of the most persistent symptoms of childhood trauma.
Relational Signs: Attachment Wounds in Adult Bonds
Fear of Abandonment
If childhood love felt unpredictable, adult love may feel like a battlefield.
Signs include:
- overexplaining
- people-pleasing
- emotional dependence
- sensitivity to criticism
- clinging in relationships
If fear of abandonment is one of the patterns you recognize in yourself, our article on healing an abandonment wound offers a gentle, deeper look at why it forms and how to soften it over time.
Fear of Intimacy
Others fear closeness just as deeply:
- shutting down when things get emotional
- difficulty expressing needs
- withdrawing after conflict
- feeling suffocated by affection
Both patterns come from the same wound: connection once felt unsafe.
Codependency
When a child learns to monitor a caregiver’s moods for safety, the adult becomes:
- the fixer
- the rescuer
- the over-functioner
- the emotional container for others
This isn’t a flaw. It was once a brilliant survival strategy.
Behavioral Signs: Avoidance, Perfectionism, and Self-Destructive Loops
Perfectionism
Perfectionism is often rooted in childhood trauma:
“If I’m perfect, I won’t be hurt.”
It can look like:
- rigid self-expectations
- harsh inner criticism
- fear of mistakes
- obsessive striving
Avoidance
Avoidance is one of the most evident signs of repressed trauma or repressed childhood memories.
It may appear as:
- chronic procrastination
- freezing under pressure
- conflict avoidance
- emotional withdrawal
Self-Destructive Behaviors
Self-destructive behaviors often appear when someone is trying to numb pain from unresolved trauma:
- substance abuse
- compulsive working
- overeating
- gaming or social media spirals
- risky sexual behavior
These behaviors overlap with several mental health disorders but originate from early traumatic experiences, not moral failure.
Physical Signs: Body Remembers What the Mind Forgot
Van der Kolk’s central idea is simple: trauma is stored in the body.
The phrase “the body keeps the score” captures the somatic nature of trauma. Adults often experience:
- chronic pain
- headaches
- digestive problems
- fatigue
- panic-like symptoms
- chest tightness
- dissociative amnesia
These physical health conditions are the legacy of a nervous system shaped by early childhood trauma. This should not be confused with weakness. It is simply a matter of how the human body adapts to danger.
How To Start Healing Childhood Trauma
Healing childhood trauma is not about forgetting traumatic experiences — it’s about learning to process trauma safely so the past stops directing your future. Healing happens through the body, brain, and relationships.
If you want a deeper, step-by-step approach to processing trauma, our article on how to heal from childhood trauma explains the complete roadmap of recovery.
Healing often requires guidance from mental health professionals who understand childhood trauma in adults and can recognize subtle signs of repressed trauma or experienced childhood trauma.
Evidence-based approaches for treating trauma include:
1. EMDR (Eye Movement Desensitization and Reprocessing)
EMDR helps reduce the emotional charge of traumatic memories. Many adults with childhood trauma symptoms benefit from this method because it works even when memories feel vague, fragmented, or repressed.
2. Cognitive Processing Therapy
This therapy focuses on identifying beliefs created during traumatic events and reframing them. It’s beneficial for adults living with post-traumatic stress disorder (PTSD).
3. Exposure Therapy
Used with care and professional support, exposure therapy helps reduce the power of triggers and avoidant behaviors.
4. Somatic Therapies (Peter Levine)
Somatic Experiencing teaches the body to complete the survival responses frozen during early childhood or traumatic events.
5. Polyvagal-Informed Practices (Stephen Porges)
Practices that activate the social engagement system help the nervous system shift out of the fight-or-flight response and into a state of safety.
6. Journaling, Mood Tracking, and Nervous System Care
Gabor Maté teaches that all coping mechanisms, even the “unhealthy” ones, are rooted in a person’s attempt to soothe emotional pain. Healing includes learning safer ways to calm the nervous system.
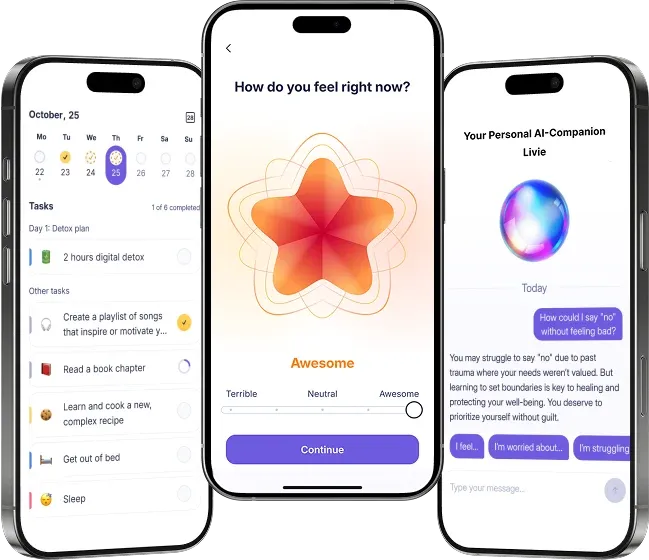
Daily mood tracking, journaling, and emotional regulation practices help you understand:
- What triggers your anxiety symptoms
- Where emotional numbness shows up
- How your body responds to stress
- When repressed memories of traumatic events surface
- How your emotional patterns shift over time
These practices help you maintain healthy relationships, build resilience, and strengthen your sense of safety. You do not have to walk this alone.
Other Supportive Tools
Healing may also involve:
- Recognizing adverse experiences from early childhood
- Learning to set boundaries
- Building supportive friendships
- Reducing substance abuse patterns
- Addressing stress and chronic pain
- Exploring spiritual or somatic practices
- Strengthening physical health through movement
- Repairing attachment wounds
- Treating co-occurring mental health disorders
Healing is not linear: some days feel like progress, others feel like reliving the past. This fluctuation is normal for adult survivors.
Your Path Forward: Personalized Healing Plan
If you want clarity on your patterns, get your personalized healing plan for childhood trauma. It gives you a custom breakdown of your emotional patterns, nervous system responses, triggers, attachment dynamics, and trauma history.
Understanding childhood trauma in adults means reclaiming agency over the present — trauma lives in the body, shaping relationships, self-worth, and physical health. Whether the trauma took the form of emotional abuse, childhood abuse, natural disasters, or subtle chronic stress, the impact is real.
But resilience is real, too. Childhood trauma survivors are not broken; they are people who adapted to overwhelming experiences in the most intelligent way their nervous system knew how. And those patterns can be healed, rewired, and softened with care and attention.
Trauma doesn’t define your future. It simply asks to be witnessed. You deserve support, safety, and a life that isn’t shaped by old survival patterns.
References
- National Center for PTSD. (n.d.). Child trauma: Prevalence and impact. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/understand/common/common_children_teens.asp
- Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. W. W. Norton & Company.
- Trauma Healing Institute. (n.d.). What is Somatic Experiencing? Foundation for Human Enrichment. https://traumahealing.org/se-101/
- Maté, G., & Maté, D. (2022). The myth of normal: Trauma, illness, and healing in a toxic culture. Avery.
- van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Penguin Books. https://www.besselvanderkolk.com/resources/the-body-keeps-the-score
- American Psychological Association. (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. https://www.apa.org/ptsd-guideline
- Centers for Disease Control and Prevention. (2022). Preventing adverse childhood experiences (ACEs). https://www.cdc.gov/violenceprevention/aces
- Cruz, D., Fortier, A. P., & Broussard, B. (2022). Developmental trauma: Conceptual framework, associated features, and implications for treatment. European Journal of Psychotraumatology, 13(1), Article 2030565. https://doi.org/10.1080/20008198.2022.2030565
FAQ: Signs of Childhood Trauma
What are the signs of childhood trauma in adults?
Can repressed childhood trauma come back later?
What causes repressed childhood memories?
What are the emotional symptoms of childhood trauma?
What physical symptoms does childhood trauma cause?
How does trauma affect relationships?
What mental health disorders can childhood trauma lead to?
How do you work with trauma from childhood?
Is substance abuse connected to childhood trauma?
Can childhood trauma affect physical health long-term?