How Anxiety Affects Your Body: The Physical Symptoms
We usually picture anxiety as endless worrying. But here’s the surprising part: anxiety is just as physical as it is mental. It can quicken your heartbeat, knot your stomach, or keep you awake at 3 AM, even when there’s no real danger.
Why does this matter? Because those physical symptoms can feel overwhelming, sometimes even similar to other health issues. The good news is that once you understand why they happen, you can use practical tools to calm your body and restore balance.
This guide will show you how anxiety affects every system in your body, which symptoms to watch, and what you can do to find relief and build resilience.
Key Learnings
- Physical symptoms can feel worrying, but occasional ones are usually harmless. When they persist, though, they can affect your well-being and lead to issues like gastritis or high blood pressure.
- Simple tools like breathing, grounding, and sleep routines can reset your nervous system.
- Tracking patterns helps you know when to self-manage or seek professional care.
The Fight-or-Flight Response
Anxiety is your nervous system flipping into survival mode, often faster than you realize. The brain’s fear center (the amygdala) scans for threats and, within milliseconds, signals the autonomic nervous system and HPA axis (the body's central stress response system). Stress hormones like adrenaline and cortisol surge, priming your body for action.
This system is ancient, designed to help humans escape predators or fight off danger. Today, though, the same wiring can kick in when you’re just facing a tough email, a crowded train, or an upcoming deadline.
What this feels like in real time:
- Heart racing to push blood toward muscles.
- Shallow breathing that leaves you dizzy or tingling.
- Muscle tension (especially jaw, shoulders, and chest).
- Heightened alertness, making noises or sensations feel sharper.
Psychologists now add “freeze” and even “fawn” to the classic “fight-or-flight” response, explaining why some people shut down or over-appease when anxious, instead of getting ready to run or fight.
Physical Symptoms by Body System
Same engine, different dashboards. Anxiety triggers the same stress response, but the way it shows up depends on which part of the body takes the hit.
Cardiovascular: Palpitations and Chest Tightness
When adrenaline surges, your heart beats harder and faster to fuel big muscles. You might feel fluttering, pounding, or skipped beats. Chest muscles also tense up, adding a sense of pressure or squeezing.
Most of the time, these sensations fade once the stressor passes. If chest pain is new, severe, or comes with fainting, shortness of breath, or exertion, treat it as a medical emergency. Anxiety may explain symptoms, but it should never stop you from ruling out heart conditions.
Respiratory: Shortness of Breath and Hyperventilation
Anxiety often speeds up breathing. You may take shallow, rapid breaths, lowering carbon dioxide levels in the blood. That drop can cause dizziness, tingling fingers, or a sense of not getting enough air.
One simple reset: lengthen your exhales. Try breathing in for four counts and out for six. This slows the stress cycle and restores balance.
Gastrointestinal: Nausea, Cramps, and IBS Flares
Anxiety disrupts gut motility, microbiome balance, and hormone signals. The result: nausea, bloating, diarrhea, constipation, or all of the above.
Research shows that more than 60% of people with irritable bowel syndrome (IBS) also experience an anxiety disorder. The connection works both ways: gut distress fuels anxiety, and anxiety worsens gut symptoms.
Neuromuscular: Tremors, Clenching, and Headaches
When your body prepares for action, muscles tighten, especially in the jaw, shoulders, and neck. Over time, this leads to tension headaches, migraines, and even grinding teeth at night.
Skin and Sensory: Sweating, Chills, and Tingling
Stress hormones also affect sweat glands and blood vessels. You might flush, sweat more than usual, or feel chills. Some people notice pins-and-needles sensations or ringing in the ears.
While unsettling, these are typically harmless signs of heightened arousal.
Anxiety and Sleep: The Vicious Cycle
Anxiety doesn’t clock out at bedtime. If anything, night is when it gets loudest. Racing thoughts, a pounding heart, or tense muscles can keep you awake or jolt you up. And once sleep is disrupted, the cycle tightens: poor rest makes your brain more reactive, which fuels even more anxiety.
Common patterns include:
- Struggling to fall asleep because thoughts won’t switch off.
- Waking often through the night.
- Early-morning awakenings with an anxious jolt.
- Night sweats or vivid, stress-fueled dreams.
Insomnia is especially common in conditions like PTSD (post-traumatic stress disorder) or panic disorder, but even everyday stress can trigger it. Over time, chronic sleep loss raises risks for heart issues, lowered immunity, and cognitive fog.
Mini Wind-Down Сhecklist
These steps create “off-ramps” for your nervous system before bed:
- Keep a consistent schedule: wake up and sleep at the same times daily.
- Build a wind-down ritual: journaling, warm shower, dim lights.
- Cut caffeine and screen time at least two hours before sleep.
- Try relaxation tools like breathing exercises or PMR we mentioned above.
Chronic Impacts of Anxiety
When anxiety becomes chronic, the body pays the price. The stress response is meant to be short-lived; when it’s “on” too often, systems wear down.
Cardiovascular Risks
Frequent adrenaline and cortisol spikes keep blood pressure elevated, stiffen blood vessels, and raise heart rate. Over time, this increases the risk of hypertension, heart disease, and even stroke. Importantly, not every flutter or chest twinge means heart disease, but ignoring symptoms can delay needed care.
Immune Function and Inflammation
Cortisol is supposed to regulate inflammation, but when it’s elevated for too long, the opposite happens. The immune system weakens, making you more prone to infections, and inflammatory conditions flare more easily.
Pain and Chronic Conditions
Muscle tension, poor sleep, and constant stress can aggravate conditions like migraines, back pain, and irritable bowel syndrome (IBS). Many people with chronic pain also report higher anxiety levels.
Long-term anxiety is a health risk factor worth taking seriously, both for your mental well-being and for the body systems that keep you alive and functioning.
Quick Wins for the Body
Think of these as nervous-system brakes you can press anytime anxiety feels overwhelming. They don’t solve the root cause, but they give your body the signal: you’re safe.
- Paced breathing. Inhale for 4 counts, exhale for 6. Within 60-90 seconds, your heart rate slows and dizziness eases.
- Grounding (5-4-3-2-1). Name 5 things you see, 4 you feel, 3 you hear, 2 you smell, 1 you taste. This shifts attention from racing thoughts to the present moment.
- Progressive Muscle Relaxation (PMR). Tense a muscle group for a few seconds, then release. Move head-to-toe. It teaches your body the difference between tension and calm.
- Light movement. A short walk, stretch, or shaking out your arms helps burn off excess adrenaline.
- Reduce triggers. Swap late-day coffee for herbal tea; replace doomscrolling with music or a podcast before bed.
Build Your Resilience Routine
Quick fixes help in the moment, but resilience comes from daily habits that keep your nervous system steadier over time. Think of it as giving your body a stronger “baseline” to return to when stress spikes.
Sleep Hygiene
- Go to bed and wake up at the same time every day (yes, even weekends).
- Keep your bedroom dark, cool, and tech-free.
- Treat winding down as a ritual: dim lights, journal, gentle stretch.
Movement that Works for You
Exercise doesn’t need to be intense. Consistent, moderate activity like a 20-minute walk, light yoga, or cycling reduces baseline anxiety levels and helps regulate sleep.
Steady Fuel
- Limit caffeine, especially after lunch.
- Watch alcohol intake, which disrupts sleep and increases anxiety rebound.
- Prioritize whole foods that stabilize blood sugar and energy.
Professional care
Sometimes habits aren’t enough. Evidence-based treatments like cognitive behavioral therapy (CBT), exposure therapy, or medication can be life-changing. Seeking help is a sign of strategy, not weakness.
When to Seek Medical Care
Most anxiety symptoms are uncomfortable but not dangerous. Still, it’s important to know when to treat them as a red flag instead of “just anxiety.”
Seek immediate medical help if you experience:
- Chest pain that feels heavy, crushing, or radiates to your arm/jaw.
- Shortness of breath that doesn’t improve with rest.
- Fainting, severe dizziness, or sudden weakness/numbness.
- New or worsening symptoms during physical exertion.
Consult a professional if:
- Anxiety symptoms are persistent or interfere with daily life.
Physical symptoms (like gut issues, migraines, or palpitations) don’t improve with self-care. - Sleep problems last more than a few weeks.
- Anxiety triggers avoidance behaviors (e.g., skipping work, social isolation).
Get urgent mental health support if you experience thoughts of self-harm or suicide. Call your local emergency number right away, or reach out to a crisis line (for example, in the U.S. dial 988).
Healthcare providers can rule out other conditions and give you strategies that make symptoms easier to manage.
Final Thoughts: Turning Awareness into Action
Your body is doing its best to protect you, even if it sometimes overshoots. And that means you can work with it: calming your breath, loosening tense muscles, building routines that steady your system.
If symptoms persist, know that help is out there. You don’t have to muscle through alone. Every small step: slower breathing, one better night of sleep, a healthier routine is training your body to remember safety. And that’s the foundation of resilience.
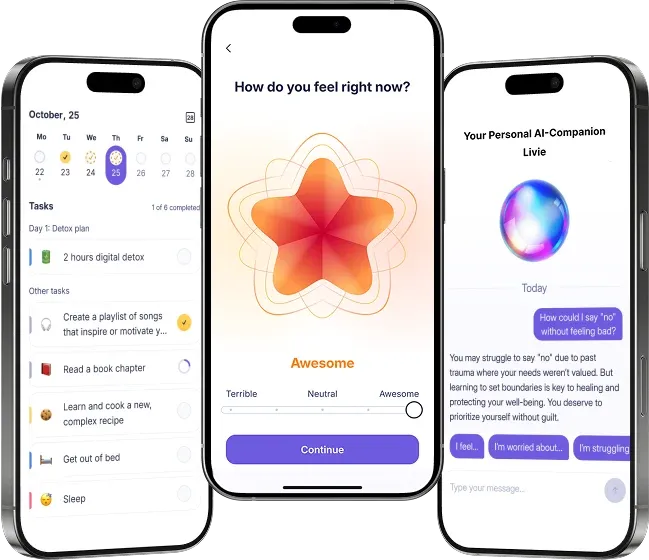
And remember: awareness is already half the job. If you’d like extra support, the Liven app can help you track symptoms, create calming routines, and reflect on your progress. Where to start? Try our anxiety test to discover your patterns and the tools that work best for you.
References
- Kaczkurkin, A. N., et al. (2020). The association between insomnia and multiple anxiety disorders in a naturalistic cognitive behavioral treatment setting. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC7369215/
- Marano, G., Traversi, G., Pola, R., Gasbarrini, A., Gaetani, E., & Mazza, M. (2025). Irritable Bowel Syndrome: A hallmark of psychological distress in women? Life, 15(2), 277. https://doi.org/10.3390/life15020277
- World Health Organization. (2025, September 8). Anxiety disorders [Fact sheet]. https://www.who.int/news-room/fact-sheets/detail/anxiety-disorders
- Cleveland Clinic. (n.d.). Hypothalamic-pituitary-adrenal (HPA) axis. https://my.clevelandclinic.org/health/body/hypothalamic-pituitary-adrenal-hpa-axis
- Simply Psychology. (n.d.). Fight, flight, freeze, fawn: The stress response explained. https://www.simplypsychology.org/fight-flight-freeze-fawn.html
- Healthline. (n.d.). High cortisol: Symptoms, causes, and treatment. https://www.healthline.com/health/high-cortisol-symptoms
- Mayo Clinic. (n.d.). Cognitive behavioral therapy (CBT). https://www.mayoclinic.org/tests-procedures/cognitive-behavioral-therapy/about/pac-20384610